Shunt closures with device are a highly effective, minimally invasive treatment option for various congenital heart defects that involve abnormal blood flow between the heart chambers or vessels. These defects, such as Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD), Patent Ductus Arteriosus (PDA), Ruptured Sinus of Valsalva (RSOV), and Aortopulmonary (AP) Window, can cause a range of symptoms and complications if left untreated. Dr. Akshat Jain, a renowned interventional cardiologist, specializes in the use of device closure techniques to treat these defects, offering patients a safer, faster recovery alternative to traditional open-heart surgery.
What Are Shunt Closures with Device?
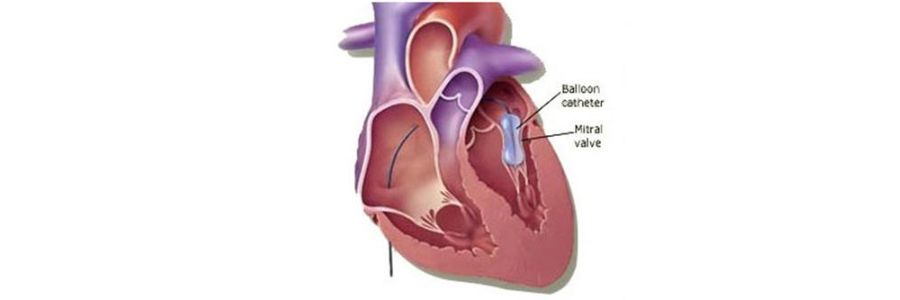
Shunt closures with device involve the percutaneous placement of a device to close abnormal openings (shunts) between the heart chambers or vessels. These devices are designed to seal off the defect, preventing blood from flowing abnormally between the left and right sides of the heart, or between the aorta and pulmonary artery, which is crucial for normal heart function.
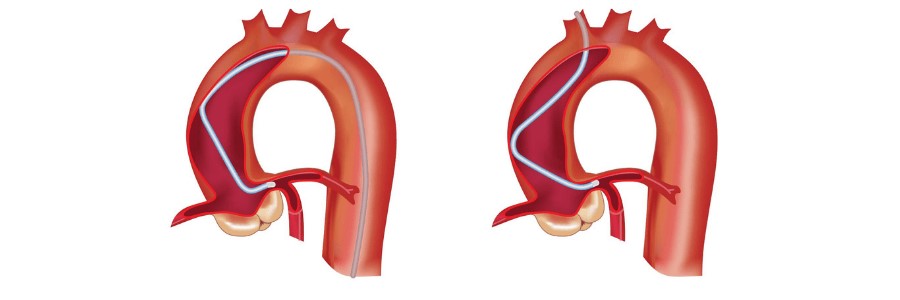
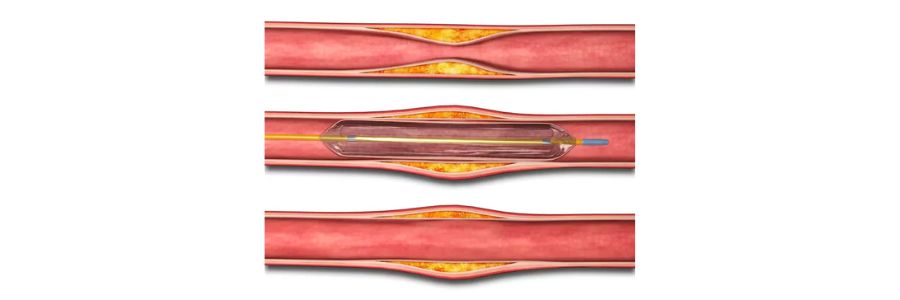
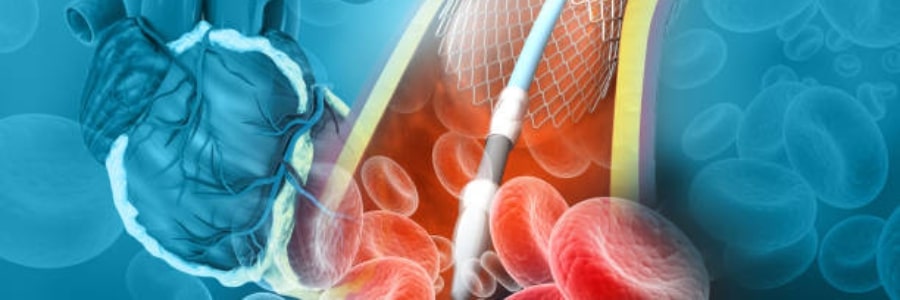
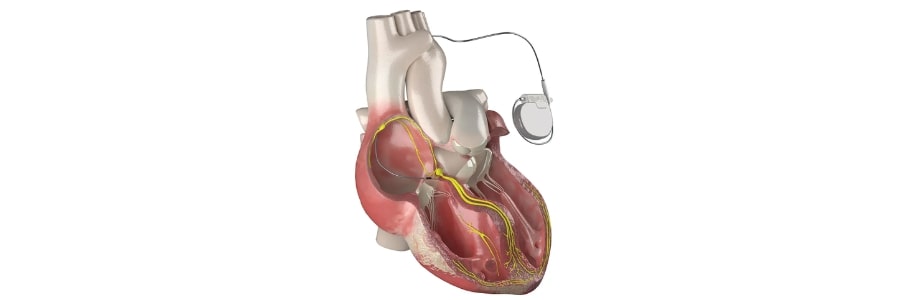
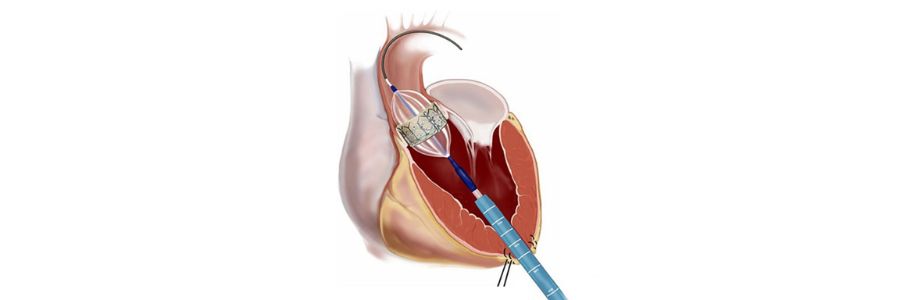
Shunt closure is typically performed using catheter-based techniques, where a device is inserted through a blood vessel (usually in the groin) and guided to the heart using advanced imaging technology like fluoroscopy and echocardiography. Once positioned correctly, the device expands to seal the defect, and over time, the body forms tissue around it, effectively closing the abnormal passage.
Types of Shunt Closures with Device
1. Atrial Septal Defect (ASD) Closure
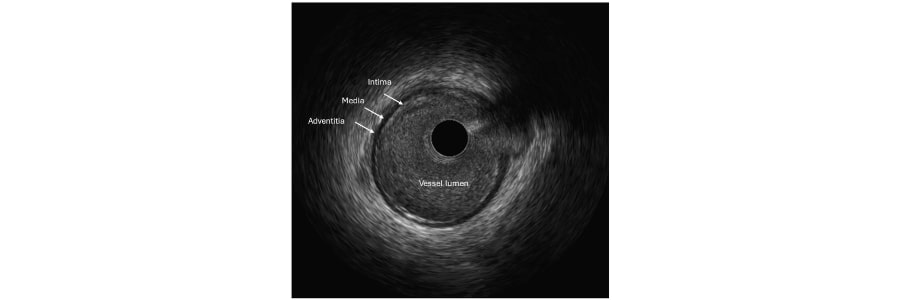
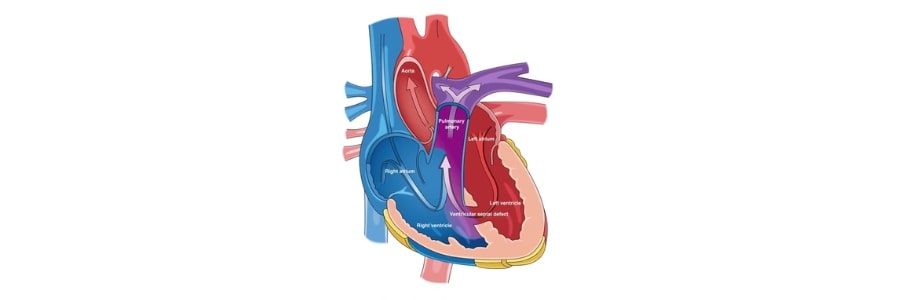
Atrial Septal Defect (ASD) is a hole in the septum (wall) that separates the left and right atria. This defect allows oxygen-rich blood from the left atrium to flow into the right atrium, leading to inefficient blood circulation. Symptoms may include fatigue, palpitations, and shortness of breath.
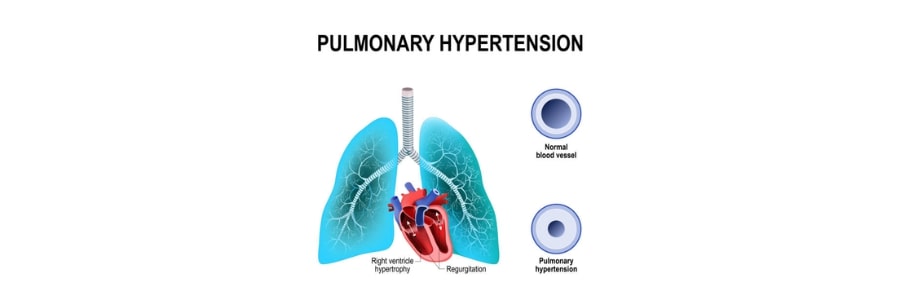
Device Closure for ASD involves using a special umbrella-like device to close the hole. This procedure can often be done with minimal sedation and is typically performed in a catheterization lab. Device closure prevents complications like stroke or pulmonary hypertension that can arise from untreated ASD.
2. Ventricular Septal Defect (VSD) Closure
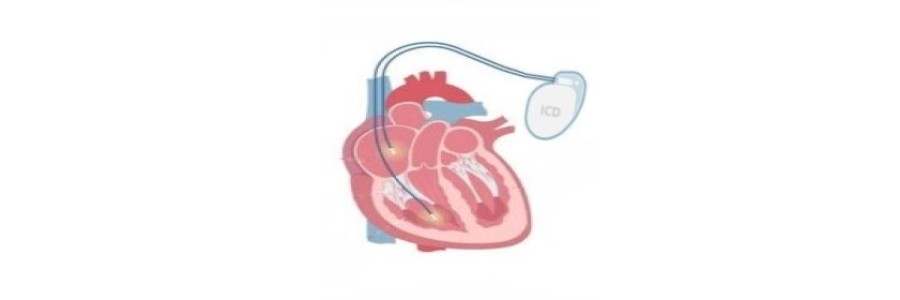
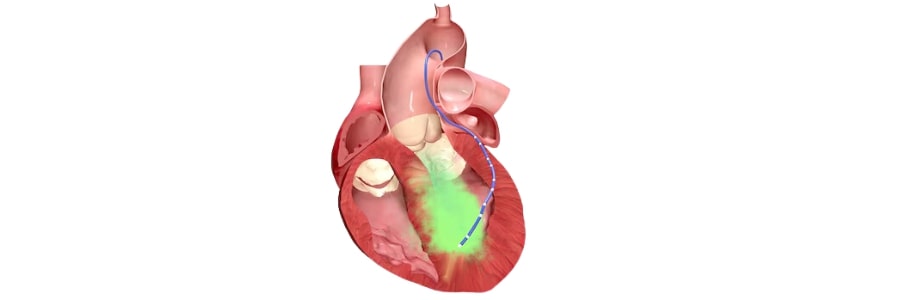
Ventricular Septal Defect (VSD) is a hole in the septum between the left and right ventricles. This defect causes oxygen-rich and oxygen-poor blood to mix, putting strain on the heart and potentially leading to heart failure or pulmonary hypertension if left untreated.
Device Closure for VSD uses a self-expanding occlusion device that is delivered via a catheter to the defect site. The device seals the VSD, preventing the abnormal blood flow and improving the heart's function.
3. Patent Ductus Arteriosus (PDA) Closure
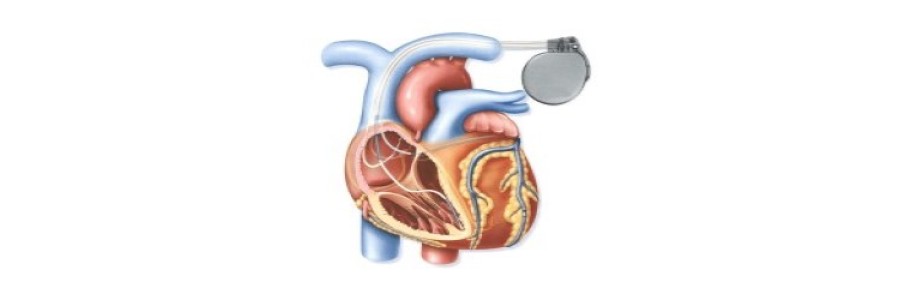
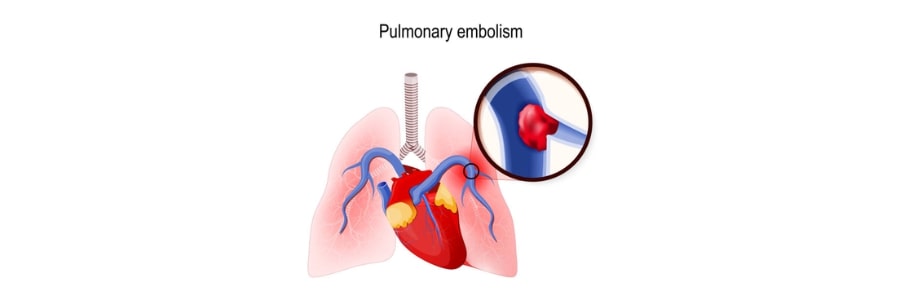
Patent Ductus Arteriosus (PDA) is a persistent opening between the aorta and the pulmonary artery that should normally close after birth. If it remains open, it can lead to excessive blood flow to the lungs, potentially causing heart failure or pulmonary hypertension.
Device Closure for PDA involves placing a coil or occlusion device to close the abnormal duct. This procedure is typically performed in infants or children, but it can also be used for adults who have an undiagnosed or untreated PDA.
4. Ruptured Sinus of Valsalva (RSOV) Closure
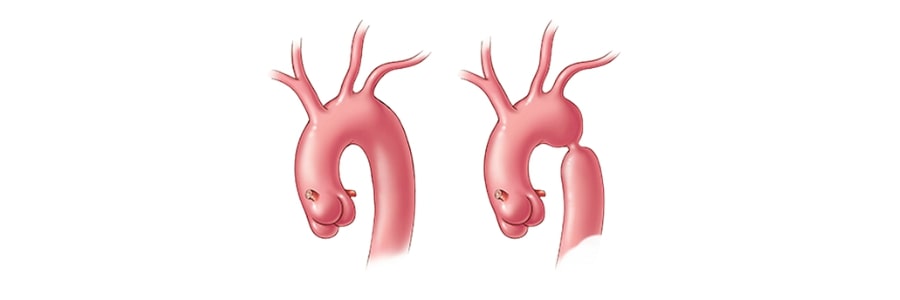
Ruptured Sinus of Valsalva (RSOV) is a rare but serious heart condition where a tear or rupture occurs in one of the sinuses of Valsalva, which are the small pockets located behind the aortic valve. This rupture allows blood to flow from the aorta into the heart chambers, typically the right atrium or ventricle, leading to symptoms like chest pain, shortness of breath, fatigue, and in severe cases, heart failure.
This condition can be congenital or acquired, often resulting from an underlying structural heart disease or trauma. If left untreated, a ruptured sinus of Valsalva can cause significant complications, including cardiac tamponade or pulmonary hypertension. Treatment typically involves surgical repair or, in some cases, endovascular procedures to close the rupture. Timely diagnosis and intervention are crucial to prevent life-threatening complications.
5. Aortopulmonary (AP) Window Closure
Aortopulmonary (AP) Window is a rare congenital defect where an abnormal connection exists between the aorta and the pulmonary artery, allowing oxygen-rich and oxygen-poor blood to mix. This condition can result in heart failure or pulmonary hypertension.
Device Closure for AP Window involves the insertion of a specialized device to close the abnormal connection. By closing this window, the procedure improves circulation and reduces strain on the heart and lungs.
Why Choose Shunt Closure with Device?
- Minimally Invasive: Shunt closure with device is a non-surgical procedure that requires only a small incision, typically in the groin, for catheter access, minimizing the need for large incisions or prolonged recovery.
- Quick Recovery: Most patients can go home within a day or two and resume normal activities after a short recovery period, with minimal pain or discomfort.
- Reduced Risk of Complications: Device closure reduces the risk of heart failure, stroke, or pulmonary hypertension, leading to better long-term health outcomes for patients.
- Effective Long-Term Results: The device, once implanted, provides a permanent solution to the defect, with high success rates and minimal risk of recurrence.
Why Choose Dr. Akshat Jain for Shunt Closure with Device?
- Expert in Interventional Cardiology: Dr. Akshat Jain is a highly skilled interventional cardiologist with years of experience in performing complex catheter-based procedures, including shunt closures.
- State-of-the-Art Technology: Dr. Jain uses the latest imaging and device technologies to perform precise and safe procedures, ensuring the best outcomes for patients.
- Patient-Centered Care: Dr. Jain tailors each treatment plan to the specific needs of the patient, ensuring personalized care and optimal results.
- Comprehensive Follow-Up: Post-procedure care is crucial for ensuring that the device is functioning correctly. Dr. Jain offers thorough follow-up to monitor recovery and heart function.
Restore Your Heart Health with Shunt Closure
If you or a loved one has been diagnosed with a congenital heart defect, shunt closure with device may provide a safe, effective solution to restore normal heart function. Dr. Akshat Jain offers advanced interventional techniques to treat ASD, VSD, PDA, RSOV, and AP Window, helping you regain optimal heart health.
Contact Dr. Akshat Jain today to learn more about this life-changing procedure and take the first step toward a healthier heart.